Medicine Operational Excellence and Transformation
The Medicine Program seized an opportunity to change process in order to improve performance and better patient care.
The Medicine Operational Excellence and Transformation (MOET) came to life in 2016 when operational excellence was identified as a priority for Providence.
Medicine, as one of our largest programs, knew that there were some areas where they were under-performing. Rather than resigning to that simply being the reality of a program of that size, Medicine stepped up to the challenge, recognizing the benefit to patients and the potential for influencing the overall Providence performance through improvement work was too great to turn away from.
“Taking a systematic look at what needed to change within the program to affect the changes that we wanted was daunting but we also knew that formalizing it and making it a Medicine-wide focus was the only way we were going to see the improved outcomes our program was aspiring to,” says Sandy Barr, program director, Medicine.
Working groups were set up at both St. Paul’s and Mount Saint Joseph hospitals to tackle this work.

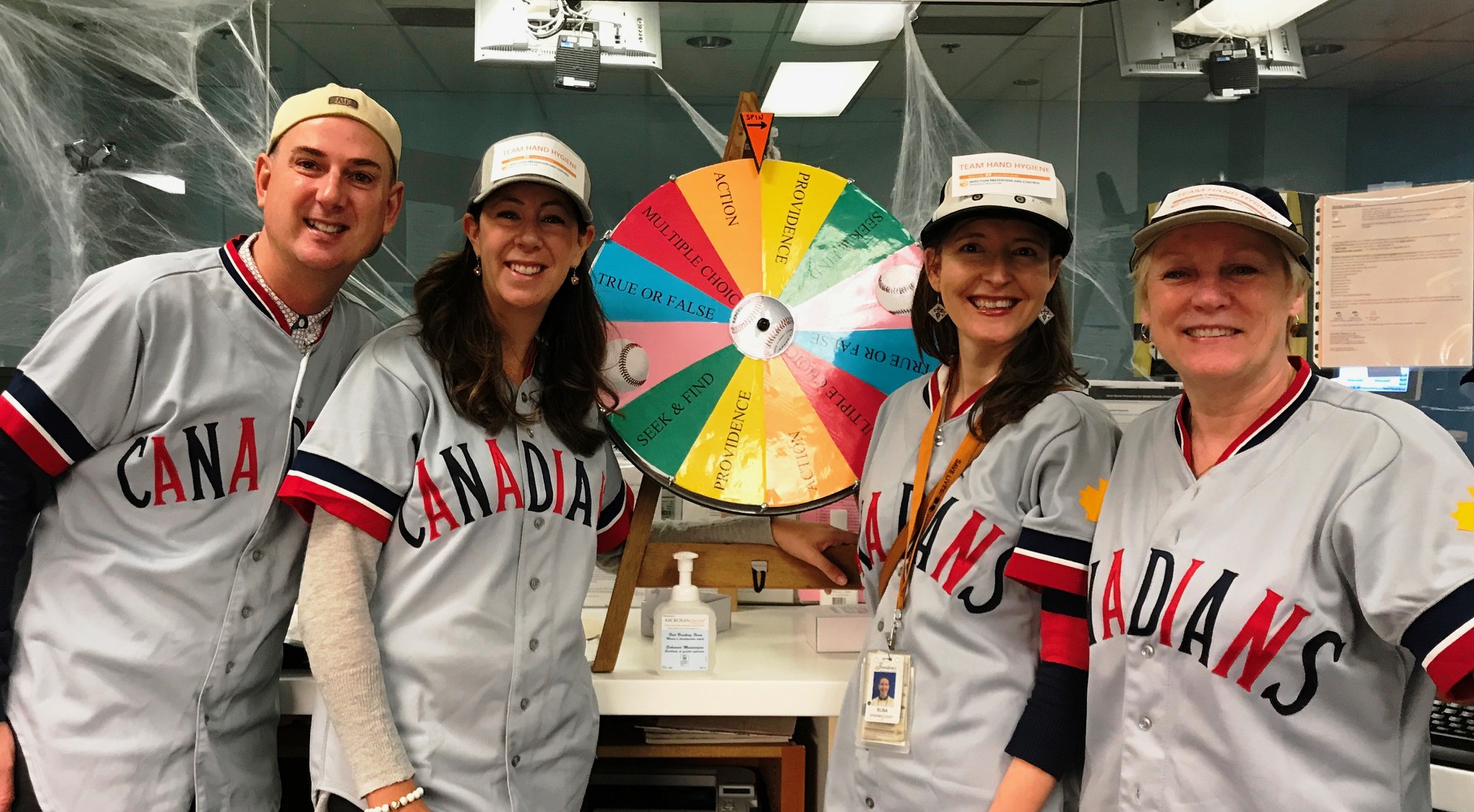
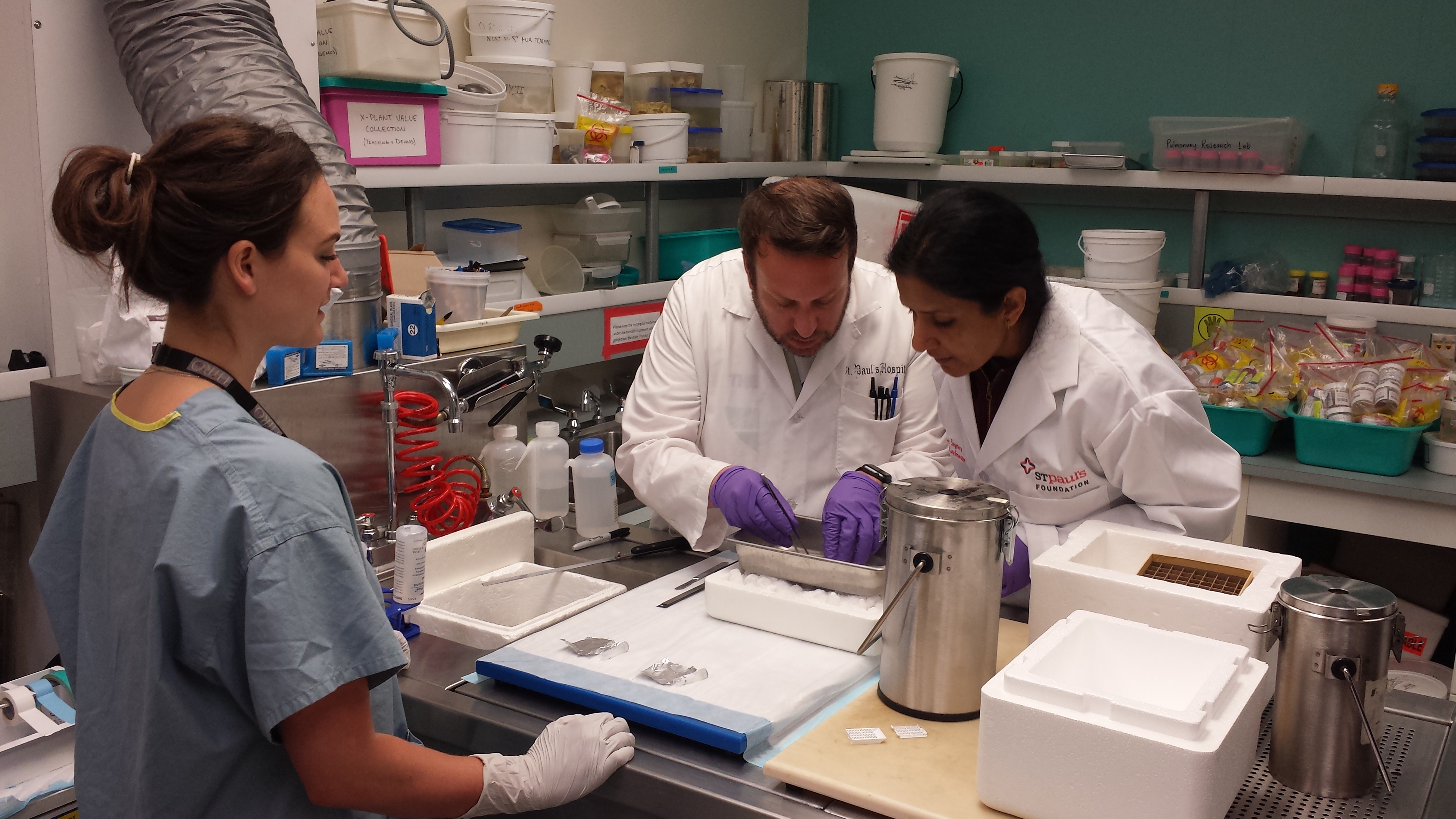
Members of the MSJ MOET working group.
A strategy not a one-off
Seen as a strategy rather than a single improvement project, the primary goal for MOET was to transform structure and processes to improve patient flow, knowing full well that improved flow would:
- Enable patients to receive the right care in the right place at the right time;
- Improve care quality and safety;
- Enhance patient and staff experience.
Putting the pieces together
Implementation of various MOET actions started in November 2016.
Guided by the best practices in “The Advisory Board Company: The Discharge Strategy Handbook” the actions were built around three change concepts:
- Estimated Discharge Date (EDD): the goal was to establish an EDD for each patient by the second day of admission as goal-post for discharge planning and patient/family communication.
- Streamline discharge planning processes and tools
- Discharge patient earlier in the day: Each patient discharged allows Medicine units to pull patients from Emergency. Early discharges enable patients to experience right care in the right place.
As a result, a large suite of changes was made:
- Implementation was staged to ensure the necessary foundation was laid first to make subsequent changes possible. The first set of improvement actions included Unit Based Teams, Geographic Clinical Teaching Unit (CTU), TeamCARE time change and Bedside Nurse at TeamCARE. They enabled EDD to be established and contributed to streamlining discharge planning process.
- Other improvement actions identified over time were informed by monitoring/audit results, stakeholder feedback and literature review. These actions included the production of a TeamCARE video for orientation of new Medicine Program staff, Criteria Led Discharge, etc.
- Stakeholders surveyed after the implementation of the initial set of actions told us that these changes greatly improved team communication and were important for improving care quality and patient flow. We have also achieved an increase in the number of patients who were able to be discharged earlier in the day, and decreased the time it takes to admit a patient following an ED visit, helping to ensure that patients are receiving the right care, in the appropriate space at the right time.
Much of this work has laid the foundation for the implementation of ongoing flow strategies on Medicine, as part of the organization’s critical area of focus on Operational Excellence.

Members of the St. Paul’s MOET working group.
Drawing on knowledge from many fields
One of the biggest successes of MOET has been one of relationships.
The project served as an opportunity to strengthen interdisciplinary communication and trust, and nurture team culture towards innovation and continuous quality improvement.
“The outcomes of this work have brought huge value, which created significant buy-in,” says Physician Program Director Dr. Anita Palepu. “Not only did that buy-in pave the way for MOET, it continues to provide opportunities for Medicine staff and medical staff to collaborate and share ideas and work together to improve current processes which, ultimately, results in improved patient care.”
MOET work was planned, implemented and monitored by an interdisciplinary Working Group with strong physician presence on each site. Patients and families were engaged throughout the initiative with initial mapping meetings being held weekly to build and sustain momentum and relationship. Everyone contributed perspectives and ideas based on their specific frame of reference, took leadership on the work related to their area, and owned the responsibility of relaying the updates and changes back to their colleagues within their respective discipline.
“MOET really shone a light on the importance of having everyone involved with a patient’s care on same page and in the same conversation. When that was realized—the impact that could be had by the right people having a conversation at the right time—changes like moving the time of TeamCARE became obvious and the benefit has been huge in terms of prioritizing work, fleshing out issues, and generally just being more efficient,” says Occupational Therapist and MOET working group member Peter Haughton.
The interdisciplinary relationship and culture strengthened everyone’s inclination toward innovation and continuous quality improvement. There was an observed shift towards openness with new ideas, the power of collaboration within a team and with other services to find better solutions, the value of embracing opportunities for changes, and the importance of owning the responsibility for achieving success.
Although the strategy has now wrapped, its sustainment has rolled into regular operations and is monitored through the Medicine Program Quality and Safety Committees. The Medicine Program and members of the MOET working group know that behaviours take time to change and that sustainability can only be attained through maintaining focus, monitoring performance, and exploring new ideas for further improvement. The Program is committed to continue this focus and effort.